Health Care Homes
Stage 1: national implementation
Commonwealth, Department of Health
The Health Care Homes program is the Australian Department of Health's (DoH) pilot program of a patient-centred healthcare model within Australia. Since 2016, AGPAL has provided the program with an ongoing package of training resources, both online and face-to-face.
This program 'trains the trainers', assisting 10 Primary Healthcare Networks (PHNs) to roll out Health Care Homes to more than 130 nominated general practices across metropolitan and regional Australia. There are currently 10,000 Australians with chronic and complex health conditions registered as a patient within the Health Care Homes program.
AGPAL's approach
How do you implement patient-centred care within the Australian healthcare system?
The DoH required a package of training resources comprising learning modules, handbook, e-learning, webinars, resources, training curriculum, and patient resources. These were to be based on Bodenheimer's 10 Building Blocks for High Performing Primary Care (10 building blocks). Also, training and support were provided to PHN team members to deliver the Health Care Homes training, known as Train the Trainer.
"We used the 10 Building Blocks as a bit of a safety net but also, combined it with two other key evidence-based of methodologies and approaches. These other were circular primary health care Patient Centred Medical Home (PCMH) model - which outlined the Safety Net Medical Home Initiative,
Safety Net Medical Home Initiative, trialled across the United States of America, and the Co-creating Health model, trialled across the United Kingdom" Dr Tina Janamian, AGPAL Health Care Homes Project Director, said. These three evidence-based courses were strategically merged into one comprehensive training package. This offered the best opportunity for successful and sustainable transformation in practices, and longer-term across the Australian healthcare system.
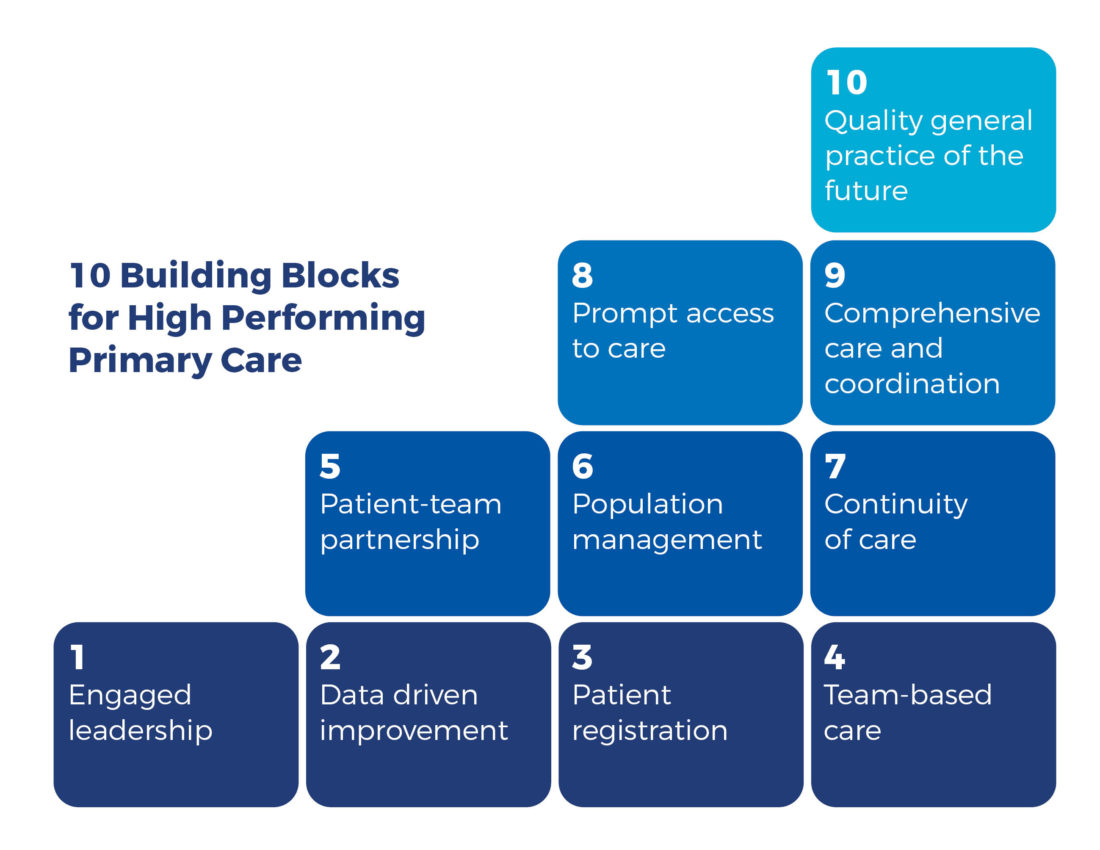
The content of the three courses complemented one another well. The 10 Building Blocks covered the elements, systems, processes and overarching structures for transformation. The co-creating Health model outlined the fundamental philosophies and approaches that are at the core of providing patient-centred care, team-based care, and enhancing patient-team partnership. The Safety Net Medical Home Initiative model focused on the necessary change tactics and tools required to support sustainable transformation and drive performance, continuous quality improvement and sustainable business operations.
By combining these three user-centred design approaches as overarching frameworks, our team developed the training material and resources required for the program. This project, split into two phases, brought together key stakeholders, industry bodies, primary health care workers and patients to develop and deliver tailored education resources fit for purpose.
The first stage was the building of the training, graphics, design, website. For this, an efficient Project Manager was on-boarded, who was skilled in both stakeholder engagement and project management due to the project's significant amounts of moving parts and differing elements.
A promising method to support primary care transformation is a practice facilitation model, which supports an ongoing, trusting relationship between an external facilitator and a primary care practice. The second stage saw the National Practice Facilitator role introduced. This ongoing role helps train and coach the practice facilitators across the 10 PHNs. The National Practice Facilitator role also assists with the mentoring, coaching, training and upskilling the PHN practice facilitators and is still ongoing throughout the project.
Developing a suite of educational resources
For the Health Care Homes project, our team co-designed suite of education and training based within a bespoke e-Learning platform.
This platform houses an array of education and training tools to support the different user groups of Health Care Homes, such as consumers, participating practices and care teams. Additional to the online resources, the team held face-to-face workshops paired with manuals to assist those working with Training the Trainers.
The co-designed suite of education and training included:
- A bespoke e-Learning platform
- 11 interactive e-learning modules
- 500 tools and resources
- 100+ activities
- 50+ training videos
- Face-to-face Train the Trainer workshops
- Train the Trainer manual
- 50+ coaching webinars
- Series of handbooks to support different user groups, and
- National coach to provide ongoing support to the practice facilitators across the participating ten PHNs.
These resources assist PHN practice facilitators to educate and train their practices in enrolling patients, shared care plans and ensured the practice is creating positive patient experiences.
Making the program a success
A key challenge that emerged and is ongoing throughout this project is the natural attrition of the PHN practice facilitator role. As a Commonwealth funded project, there is a cyclical requirement for continuing training and support to incoming PHN practice facilitators.
When trained, and provided adequate time within the role for their Health Care Homes practices, a PHN practice facilitator has the opportunity to champion the project. These champions have shown that predictions and aims of the project can be achieved with the right personnel, time allocation and resources.
PHN practice facilitators who champion the project regularly visit their participating Health Care Homes practices, check-in digitally, assist with training and implementing changes and provide ongoing support. This high-level support, provision of tools and resources has been the difference between a general practice becoming a successful Health Care Home practice.
While 10 PHNs are participating in the Health Care Homes project, there are an additional 21 PHNs who received Commonwealth funding to implement trial person-centred care approaches. Our Education and Training Team welcomed the opportunity to assist these PHNs.
Although their principles and approaches were similar, these these 21 PHNs have created innovative models and ideas that have had significant learning opportunities for the model as a whole. Various training types have been created and implemented, relevant to patient-centred care, that assists general practices not to be left behind should Health Care Homes nationally roll-out.

Alexis Mohay
Director
Health Care Homes
"AGPAL consistently demonstrated their expertise and responsiveness throughout the development process.
AGPAL met delivery time frames throughout the project and have been accommodating in responding to program and policy changes and continues to be a valuable partner in implementing the Health Care Homes program."
Patient-centred care in Australia
"One in four Australians have at least two chronic health conditions. These people need services from a number of health professionals working in different locations. A Health Care Home is a general practice or Aboriginal Community Controlled Health Organisation (ACCHOs) that coordinates care for patients with chronic and complex conditions."1
In 2016 the DoH began the process of working towards transforming Australia's primary health care system by improving the provision of care for people with chronic and complex conditions. The solution was to trial what is now known as the Health Care Homes model. An evidence-based, coordinated, model of care that provides doctors, nurses, allied health and other healthcare professionals greater flexibility to shape care around an individual patient's needs and encourages patients to participate in and direct their own care.
By mid-2016, the DoH began the process of requesting the development of a suite of educational resources for general practices and Aboriginal Medical Services to assist practices to commence a Health Care Homes trial.
The program aimed to assist patients, carers and their families in providing a coordinated care approach with their various healthcare professionals to overcome communication challenges within their healthcare journey. This approach not only kept the patient at the centre of the plan but also reduced the risk for their treatment.
The Government announced that AGPAL Group of Companies and their partners were awarded this tender in late 2016. The program launched in 2018 and runs through until 30 June 2021.
A passionate public health advocate
To spearhead this project, AGPAL sought the experience and expertise of Dr Tina Janamian. Dr Janamian has an impressive list of qualifications including a Doctorate of Philosophy (PhD), Public Health, Master of Medical Science, Public Health (research) and Master of Business Administration (MBA). Adding to this is a Bachelor of Science, Biochemistry and biological sciences and a Graduate Diploma, Executive Leadership.
A vast majority of this recent academic background was based around primary care tools and resources, innovative models of care, policies and practice, and was complemented with recent experience in similar projects.3,4,5,6
Dr Janamian didn't set out for a career in public healthcare reform, her goal originally was something more clinical. However, after completing her Bachelor of Science, Dr Janamian explored what motivated her.
"I wanted to make a difference in Australia's health system, to be able to treat patients as individuals, as a person. My whole philosophy about healthcare is around person-centred care, so being able to address the patient and their family's needs. I thought, how can I do this without being a clinician?
That led me to the path of doing a Masters and PhD in Public Health, which looks at primary care across the spectrum and trying to work with practices and policymakers to make a difference in everyone's lives and improve the health of the community" she continued.
Over the past two decades, Dr Janamian has worked extensively on projects focused on patient-centred care. One project investigated the quality of care between the interface of primary and secondary care, so the transition of a patient through primary to secondary and back again - and aimed to improve this cycle. Another project involved supporting chronic disease patients with their management by empowering self-care for more than ten years.
A different, larger-scale project, was with four hospital outpatient departments and a variety of their staff and other internal departments. Working together these teams tried to reduce waitlist times, and empower the patients to take care of themselves so they were not on waitlists. These projects, along with her network of international colleagues working on similar patient-centred care models around the world, made Dr Janamian the perfect fit to lead AGPAL's Health Care Homes team.
For Dr Janamian, the best moments through the Health Care Homes project has been watching light bulb moments happen for the health care workers implementing the program.
"They (the clinicians) read it, they see it, but they don't fully understand it. Then they have a patient, or something happens, and they have that light bulb moment. They get to a point and say 'oh that's what we're trying to do!' or 'that's what we're trying to do here'" said Dr Janamian.
"I've seen that in several people, and then they share stories where they tell colleagues I did this or that and was able to make a difference. It almost sparks a new lease on what they're doing or reminds them of why they became a GP in the first place" Dr Janamian explained.
References
- Janamian, T., Jackson, C., Glasson, N. and Nicholson, C., 2014. A systematic review of the challenges to implementation of the patient‐centred medical home: lessons for Australia. Medical Journal of Australia, [online] 201(S3). Available at: https://www.mja.com.au/journal/2014/201/3/systematic-review-challenges-implementation-patient-centred-medical-home-lessons [Accessed 11 November 2020].
- Janamian, T., Upham, S., Crossland, L. and Jackson, C., 2016. Quality tools and resources to support organisational improvement integral to high‐quality primary care: a systematic review of published and grey literature. Medical Journal of Australia, [online] 204(S7). Available at: https://www.mja.com.au/journal/2016/204/7/quality-tools-and-resources-support-organisational-improvement-integral-high [Accessed 7 November 2020].
- Upham, S., Janamian, T., Crossland, L. and Jackson, C., 2016. A Delphi study assessing the utility of quality improvement tools and resources in Australian primary care. Medical Journal of Australia, [online] 204(S7). Available at: https://www.mja.com.au/journal/2016/204/7/delphi-study-assessing-utility-quality-improvement-tools-and-resources-australian [Accessed 11 November 2020]
4. Janamian, T., Jackson, C., Glasson, N. and Nicholson, C., 2014. A systematic review of the challenges to implementation of the patient‐centred medical home: lessons for Australia. Medical Journal of Australia, [online] 201(S3). Available at: https://www.mja.com.au/journal/2014/201/3/systematic-review-challenges-implementation-patient-centred-medical-home-lessons [Accessed 11 November 2020].
5. Janamian, T., Upham, S., Crossland, L. and Jackson, C., 2016. Quality tools and resources to support organisational improvement integral to high‐quality primary care: a systematic review of published and grey literature. Medical Journal of Australia, [online] 204(S7). Available at: https://www.mja.com.au/journal/2016/204/7/quality-tools-and-resources-support-organisational-improvement-integral-high [Accessed 7 November 2020].
6. Upham, S., Janamian, T., Crossland, L. and Jackson, C., 2016. A Delphi study assessing the utility of quality improvement tools and resources in Australian primary care. Medical Journal of Australia, [online] 204(S7). Available at: https://www.mja.com.au/journal/2016/204/7/delphi-study-assessing-utility-quality-improvement-tools-and-resources-australian [Accessed 11 November 2020]
